1. Gavin NC, Webster J, Chan, RJ, Rickard
CM. Frequency of dressing changes for central venous access devices on catheter-related infections.
Cochrane Database of Systematic Reviews 2016. Issue 2. Art. No.: CD009213. DOI: 10.1002/14651858.
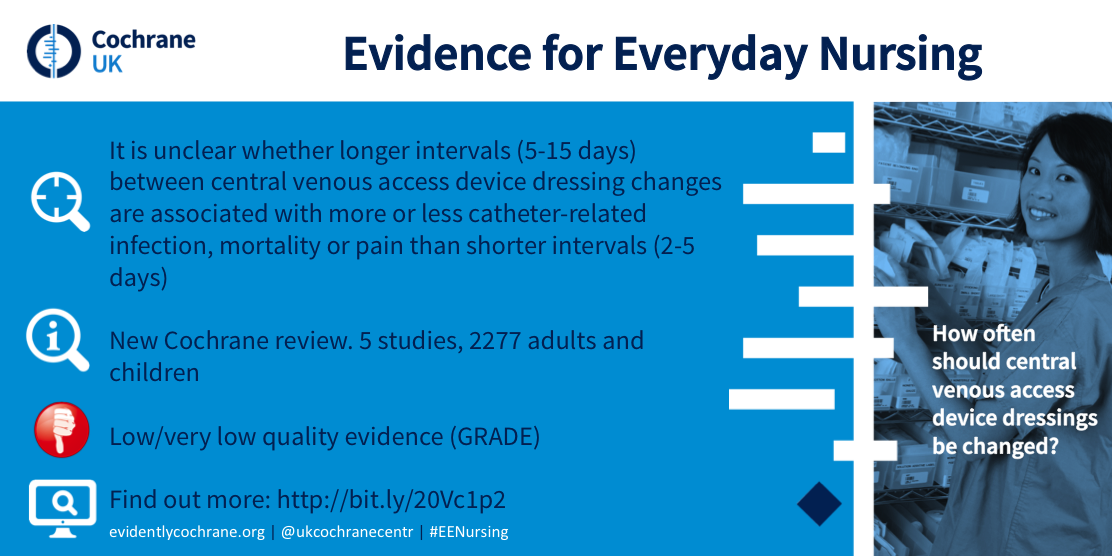
We reviewed the available evidence about the effect of different time intervals between dressing
changes for CVADs and whether they had an effect on the risk of CRBSI and other complications. We found
five studies that provided information for our review. The best available evidence is currently inconclusive
regarding whether longer intervals between CVAD dressing changes are associated with more or less catheter-related
infection, mortality or pain than shorter intervals.
http://www.cochrane.org/CD009213/WOUNDS_how-often-should-dressings-central-venous-access-devices-cvads-be-changed-reduce-catheter-related
2. Choudhury MA, Marsh N, Banu S, Paterson DL, Rickard CM, McMillan D. Molecular comparison
of bacterial communities on peripheral intravenous catheters and matched skin swabs. PloS One. 2016:
11(1) e0146354.
This study aimed to determine the bacterial community structures on skin
at PIVC insertion sites and to compare the diversity with associated PIVCs. Diverse bacterial communities
were observed at skin sites despite skin decolonization at PIVC insertion. The positive association of
skin and PIVC tip communities provides further evidence that skin is a major source of PIVC colonisation
via bacterial migration but microbes present may be different to those traditionally identified via culture
methods. The results provide new insights into the colonisation of catheters and potential pathogenesis
of bacteria associated with CRBSI, and may assist in developing new strategies designed to reduce the
risk of CRBSI.
http://www.plosone.org/article/fetchObject.action?uri=info:doi/10.1371/journal.pone.0146354&
representation=PDF
3. Bugden S, Shean K, Scott M, Fraser JF, Mihala G, Clark S, Johnstone
C, Rickard CM. Skin glue reduces the failure rate of emergency department inserted peripheral intravenous
catheters: A randomized controlled trial. Annals of Emergency Medicine. 2015. Early on-line.
Peripheral intravenous catheters are the most common invasive device in health care yet have
very high failure rates. We investigated whether the failure rate could be reduced by the addition of
skin glue to standard peripheral intravenous catheter care. Methods: We conducted a single-site, 2-arm,
nonblinded, randomized, controlled trial of 380 peripheral intravenous catheters inserted into 360 adult
patients. The standard care group received standard securement. The skin glue group received standard
securement plus cyanoacrylate skin glue applied to the skin insertion site. The primary outcome was peripheral
intravenous catheter failure at 48 hours, regardless of cause. Secondary outcomes were the individual
modes of peripheral intravenous catheter failure: infection, phlebitis, occlusion, or dislodgement. Results:
Peripheral intravenous catheter failure was 10% lower (95% confidence interval 18% to 2%; P=02) with skin
glue (17%) than standard care (27%), and dislodgement was 7% lower (95% confidence interval 13% to 0%;
P=04). Phlebitis and occlusion were less with skin glue but were not statistically significant. There
were no infections. Conclusion: This study supports the use of skin glue in addition to standard care
to reduce peripheral intravenous catheter failure rates for adult emergency department patients admitted
to the hospital.
http://www.annemergmed.com/article/S0196-0644(15)01535-8/pdf
4. Carr, P, Rippey J, Budgeon C, Higgins NS, Cooke ML, Rickard CM. Insertion of peripheral
intravenous cannulae in the Emergency Department: Factors associated with first-time insertion success.
Journal of Vascular Access. ePublished, Dec 2015.
We sought to identify the reasons for
peripheral intravenous cannulae (PIVC) insertion in the emergency department (ED), and the first-time
insertion success rate, along with patient and clinician factors influencing this phenomenon. Methods:
A prospective cohort study of patients requiring PIVC insertion in a tertiary ED. A total 734 PIVC insertions
were included in the study where 460 insertions were analysed. The first-time insertion success incidence
was 86%. The antecubital fossa (ACF) site accounted for over 50% of insertions. Multivariate logistic
regression modelling to predict first-time insertion success for patient factors found: age <40 versus
80+ years, emaciated versus normal patient size, having a visible or palpable vein/s, and ACF versus forearm
insertion site to be statistically significant. Statistically significant clinician factors predicting
success were: higher number of prior cannulation procedures performed, and increased clinician perception
of the likelihood of a successful insertion. When patient and clinician factors were combined in a logistic
regression model, emaciated versus normal, visible vein/s, ACF versus forearm site, higher number of prior
PIVC procedures performed and increased clinician perceived likelihood of success were statistically associated
with first-time insertion success.Conclusion: PIVC insertion success could be improved if performed by
clinicians with greater procedural experience and increased perception of the likelihood of success.
5. Takashima M, Ray-Barruel G, Keogh S, Rickard CM. Randomised controlled trials in
peripheral vascular access catheters: a scoping review. Vascular Access. November 2015: 1(2); 10-37.
Randomised controlled trials (RCTs) are the "gold standard" for evaluating effectiveness
of interventions, as they provide the most reliable evidence with minimal bias compared to other study
designs. However, if the number and quality of RCTs are poor, studies may give inconsistent results and
small effect sizes, creating difficulties in generalising the findings to a broader population. This scoping
review investigated the current evidence for the insertion and management of peripheral vascular devices,
including intravenous, midline, and arterial catheters. We searched Pubmed, Cochrane Central Register
of Controlled Trials, and CINAHL between 1 January 2005 and 30 June 2015. The final review included 128
RCTs (94 peripheral intravenous catheters, 2 midline catheters, and 32 arterial catheters). Catheter insertion
strategies and analgesia methods have been comprehensively studied, particularly for peripheral intravenous
catheters, but more RCTs are needed to address post-insertion care and maintenance, including dressings
and securement, flushing practices and infection prevention strategies such as skin preparation and hub
decontamination. This peripheral vascular catheter scoping review will enable clinicians and researchers
to identify the gaps in evidence and prioritise areas needing further research.
http://s3-ap-southeast-amazonaws.com/wh1.thewebconsole.com/wh/4798/images/Takashima-2015.pdf
6. Evans O, Gowardman J, Rabbolini D, McGrail M, Rickard CM. In situ diagnostic methods for
catheter related bloodstream infection in burns patients: A pilot study. 2016 Jan 5. pii: S0305-4179(15)00203-X.
doi: 10.1016/j.burns.2015.07.004.
Aims: To assess the sensitivity, specificity
and accuracy of two in situ diagnostic methods for CR-BSI in an adult ICU burns population: Differential
Time to Positivity (DTP) and Semi-Quantitative Superficial Cultures (SQSC).
Conclusion:Both DTP
and SQSC displayed high specificity, NPV and accuracy in a population of adult burns patients. These features
may make these tests useful for ruling out CR-BSI in this patient group. This study was limited by a low
number of events and further research is required.
http://www.ncbi.nlm.nih.gov/pubmed/26778703
7. Peter J Carr, James C R Rippey, Marie L Cooke, Chrianna Bharat, Kevin Murray, Niall S Higgins,
Aileen Foale, Claire M Rickard. Development of a clinical prediction rule to improve peripheral intravenous
cannulae first attempt success in the emergency department and reduce post insertion failure rates: the
Vascular Access Decisions in the Emergency Room (VADER) study protocol. BMJ Open 2016;6:2 e009196
doi:10.1136/bmjopen-2015-009196
Summary: The findings of our study will provide new evidence
to improve insertion success rates in the ED setting and identify strategies to reduce premature device
failure for patients admitted to hospital wards. Results will unravel a complexity of factors that contribute
to unsuccessful PIVC attempts such as patient and clinician factors along with the products, technologies
and infusates used.
http://www.ncbi.nlm.nih.gov/pubmed/26868942
|